Plantar Fasciitis

Plantar fasciitis, also known as "runner's foot," is a common condition, more prevalent in women than men. Patients with this condition experience sharp pain in the heel upon getting out of bed in the morning or standing up after prolonged sitting. Walking, even just a few steps, can be extremely painful.
What is plantar fasciitis?
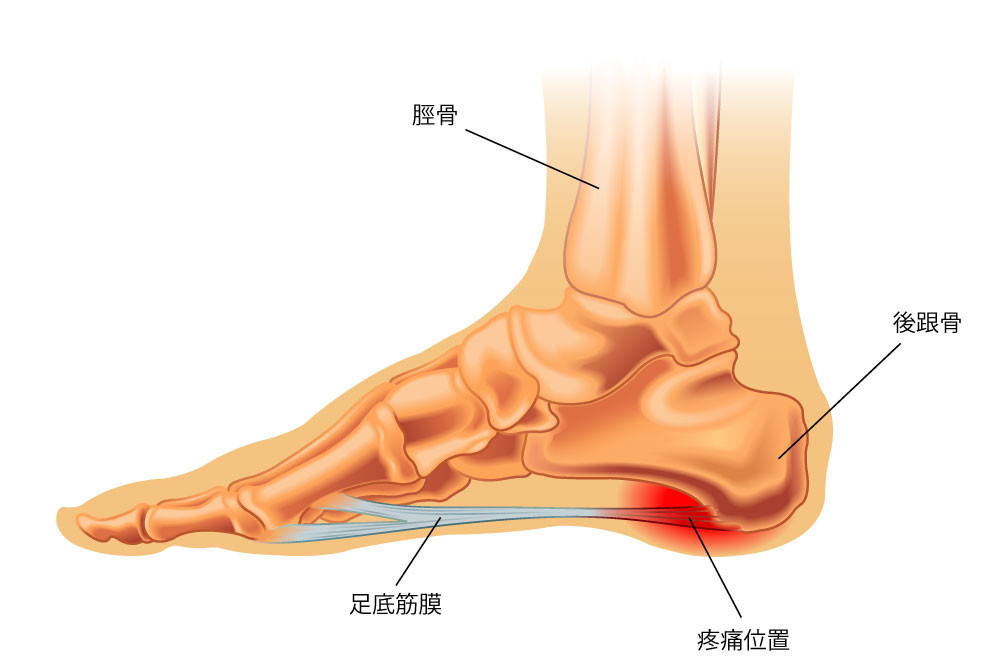
The plantar fascia is a thick, soft tissue that lies above the muscle layer and beneath the bottom layer of fat in the sole. It connects the forefoot to the heel bone and plays a role in supporting the arch of the foot and maintaining joint stability. When we stand, walk, climb stairs, or run, there is a certain amount of load on the arch of the foot, which causes the plantar fascia to be stretched. If there is a sudden increase in load on the plantar fascia or if it undergoes prolonged stretching over time, the end connecting to the heel bone can become inflamed or even torn, resulting in heel pain.
Symptoms of plantar fasciitis
Common symptoms of plantar fasciitis include:
- Stabbing pain in the bottom of the foot or heel, especially upon getting out of bed or standing up after prolonged sitting.
- The pain decreases gradually after walking for a while or covering a certain distance.
- Some severe cases may experience renewed pain after walking for an extended period.
- The pain may radiate from the heel to the arch of the foot or toes.
Who is at risk for plantar fasciitis?
- People with prolonged walking or standing, such as athletes, teachers, and salespersons.
- Sports enthusiasts, especially those involved in high-impact activities like running, basketball, tennis, etc.
- Obese individuals, as excess weight increases the pressure on the plantar fascia and raises the likelihood of developing plantar fasciitis.
Does wearing high heels increase the risk of plantar fasciitis?
Wearing high heels can increase the risk of developing plantar fasciitis. High heels alter the biomechanics of the feet, placing excessive strain on the plantar fascia. This can lead to inflammation and injury, making individuals who frequently wear high heels more susceptible to developing plantar fasciitis. Choosing supportive and comfortable footwear is advisable to reduce the risk of this condition.

Does having flat feet lead to plantar fasciitis?

Even runners with flat feet do not necessarily develop plantar fasciitis from running. Although flat feet can cause the fascia to stretch, there are other factors to consider:
Firstly, the elasticity of the fascia. Even though the arch of the foot may collapse and stretch the fascia with each impact while running, if it has good elasticity, it can stretch and quickly return to its original state without being easily damaged.
Secondly, the support provided by the muscles of the foot. If the muscles that support the arch of the foot are strong, they can assist in maintaining the arch, stabilising the foot, and propelling the stride while running. This can compensate for the inherent limitations of flat feet.
Both of these factors can be improved with effort. Heat therapy and appropriate massage techniques can enhance the elasticity of the fascia, while exercises targeting the intrinsic muscles of the foot, such as towel scrunches, can be beneficial. Furthermore, wearing suitable running shoes with arch support and using orthotic inserts can assist runners with flat feet protect the fascia and reduce the risk of developing plantar fasciitis.

How do doctors diagnose plantar fasciitis?
Orthopaedic doctors diagnose plantar fasciitis by taking a careful medical history from the patient, including information about the duration, severity, activity habits, and potential pain triggers. They also rule out other possible conditions. Following the medical history, a clinical examination is conducted. Plantar fasciitis commonly causes pain in the heel region, and the patient's tender spot is typically found on the underside of the foot. The doctor will perform a pressure test using their thumb, applying pressure to specific areas of the plantar fascia, particularly the attachment point near the heel, to determine if it causes pain. If the patient experiences pain during the test, it indicates typical plantar fasciitis.

In some cases, doctors may recommend imaging tests such as X-rays, ultrasound, or magnetic resonance imaging (MRI) to rule out other possible conditions, such as fractures or other tissue injuries. However, in most cases, the diagnosis of plantar fasciitis can be determined based on the patient's medical history and clinical examination. The doctor will consider all these factors together to make an accurate diagnosis.
Some patients may misunderstand that the purpose of X-rays is to check for the presence of bone spurs. However, around 50% of individuals in the general population may have bone spurs even without any symptoms. Therefore, orthopaedic doctors generally consider that bone spurs are not the primary cause of plantar fasciitis.
How is plantar fasciitis treated?
The treatment of plantar fasciitis typically involves several approaches:
Medication: Doctors may prescribe anti-inflammatory and pain-relieving medications to alleviate pain and inflammation. These medications can include non-steroidal anti-inflammatory drugs (NSAIDs) or topical anti-inflammatory creams.
Physiotherapy: One of the main goals of physical therapy is to stretch the Achilles tendon at the back of the lower leg to relieve symptoms of plantar fasciitis. Physiotherapists may use massage, stretching exercises, hot and cold therapy, and other modalities to reduce pain, promote blood circulation, and aid recovery.
Shockwave therapy: Shockwave therapy is a non-invasive treatment widely used to manage plantar fasciitis. It involves the delivery of high-energy sound waves to the affected area through the skin, which may help improve blood supply and elasticity of the fascia. The specific mechanisms of shockwave therapy are still being studied, and further research is needed.
Exercise therapy: Exercise therapy focuses on strengthening the lower leg muscles and improving flexibility. Physical therapists can develop specific exercise plans to strengthen the calf muscles and reduce the burden on the plantar fascia.
For most patients, symptoms can be alleviated within eight to nine weeks through a combination of medication, physical therapy, and exercise therapy. However, in cases where conservative treatments do not result in improvement, surgery may be considered. It is important to note that surgical intervention is only necessary for a small number of patients who do not respond to conservative treatments, and the majority of patients do not require surgery.
Our Team
Virtus Medical Orthopaedics & Traumatology Specialists
More:
-
Specialty Services - Orthopaedics & Traumatology
-
Physiotherapy Services - Physiotherapy