Endometrial Polyps
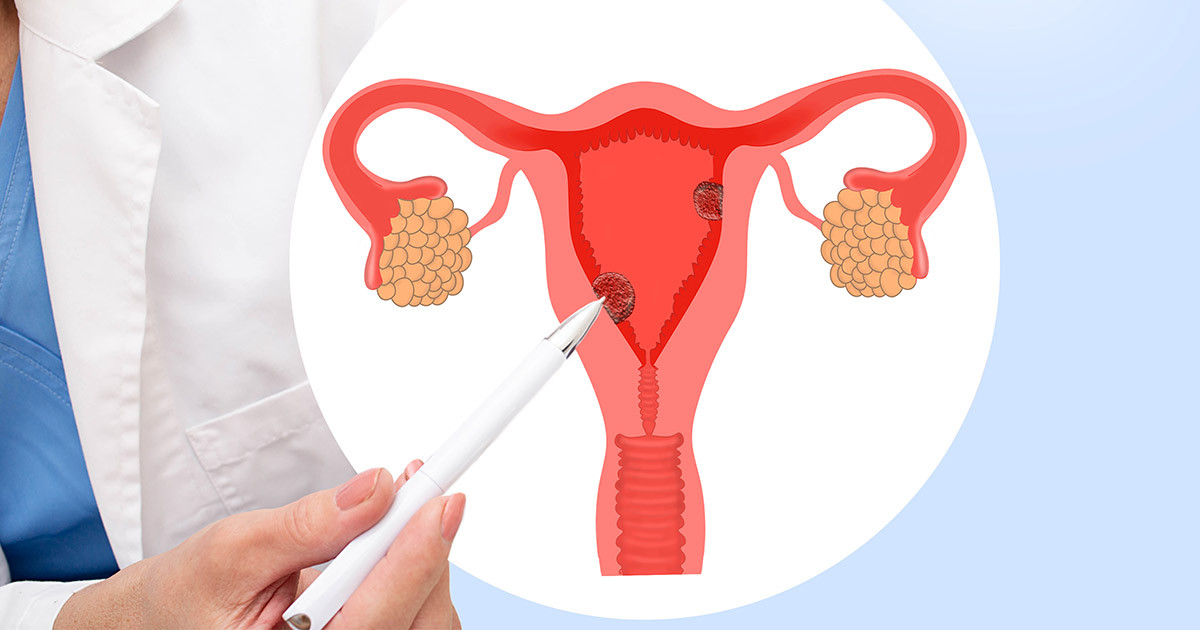
What are endometrial polyps?
Endometrial polyps are benign tumours that result from the excessive growth of endometrial cells in the innermost layer of the uterus, where the embryo implants during pregnancy. Endometrial polyps are quite common in clinical practice and can occur as single or multiple growths. The symptoms of patients with endometrial polyps are often not apparent and are typically diagnosed through regular ultrasound examinations or hysteroscopy for infertility investigations. The exact cause of endometrial polyps in most patients is unknown, but it is often believed to be associated with the following factors:
-
Elevated estrogen levels can be caused by obesity or the use of medications for breast cancer treatment (such as tamoxifen).
-
Chronic inflammation.
Who is at a higher risk for endometrial polyps?
Women between the ages of 30 and 50 are more likely to develop endometrial polyps than younger women. Postmenopausal women also have a chance of developing endometrial polyps, although it is extremely rare for patients aged 20 or below in clinical practice.
What are the symptoms of endometrial polyps?
Common symptoms include irregular menstrual cycles, heavy menstrual bleeding, prolonged periods, bleeding between periods, and postmenopausal bleeding. Endometrial polyps can also interfere with embryo implantation and, in severe cases, lead to infertility.
How is endometrial polyps diagnosed?
The doctor will inquire about your menstrual history, including dates, flow, and abnormal bleeding. Diagnostic tests that the doctor may perform include:
Transvaginal ultrasound
This method is more suitable for sexually active women and provides higher accuracy compared to abdominal ultrasound. Before the examination, you will need to empty your bladder and relax. The doctor will insert a slender probe into the vagina to obtain precise images of the uterus and ovaries. The optimal time for this examination is after the menstrual period and before ovulation, as the endometrium is thinner after the menstrual blood is cleared, making it easier to detect small polyps.

Hysterosalpingography
This involves injecting physiological saline into the uterus while performing an ultrasound to increase the sensitivity and specificity of the detection.
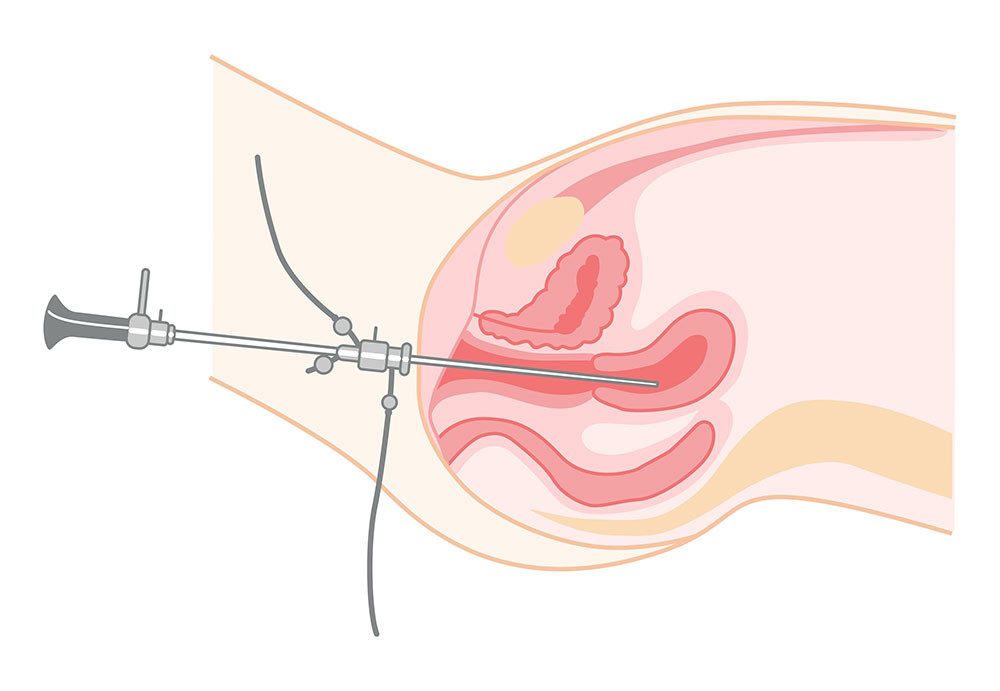
Hysteroscopy
This procedure involves inserting a thin tube with a camera (hysteroscope) through the vagina and cervix to visually examine the uterus's inside. It can be performed under general anaesthesia or local anaesthesia.
Endometrial biopsy
An endometrial biopsy aids in diagnosing abnormalities in the uterine cavity and can be performed in an outpatient setting without hospitalization. During the procedure, the doctor will insert a tube through the vagina and cervix into the uterine cavity to collect a sample of the endometrial tissue for laboratory analysis.
Dilation and curettage (D&C)
D&C is a surgical procedure to remove and sample the endometrial tissue from the uterus for diagnostic purposes. It can be performed concurrently with other procedures, such as hysteroscopy. If polyps or fibroids are discovered during the surgery, the doctor may remove them simultaneously.
Treatment of endometrial polyps
Surgical removal is currently the most effective and direct method of treating endometrial polyps, although there is still a possibility of recurrence after the procedure.
Hysteroscopic polypectomy
This procedure is performed using a hysteroscope to remove smaller endometrial polyps. It can help alleviate symptoms such as abnormal vaginal bleeding and excessive menstrual flow.
Our Team
Virtus Obstetrics and Gynaecology specialists
-
Specialty Services - Obstetrics and Gynaecology