Asthma

About Asthma
Asthma is a common lower respiratory disease which affects about 5% of the population. In Hong Kong, asthma leads to several thousand hospitalizations every year. In 2016, there were 113 registered deaths caused by asthma, of which 30% aged below 65 years old.
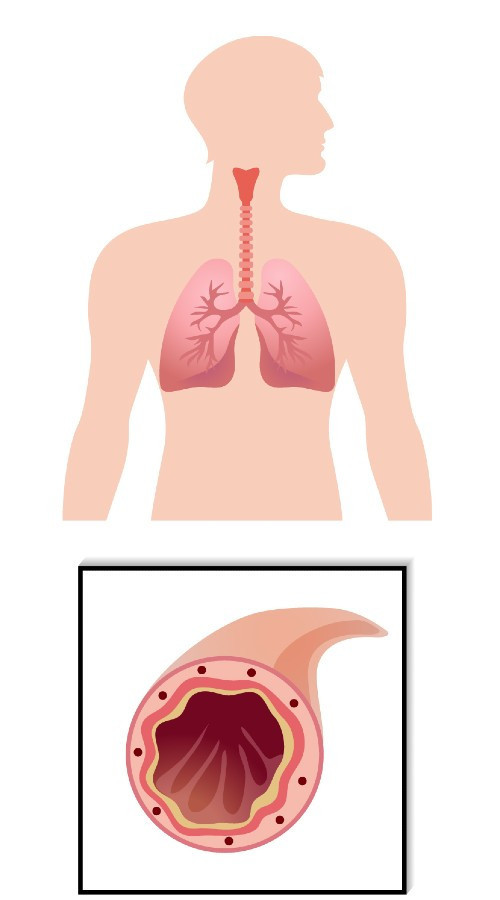
Normal Bronchial Tube
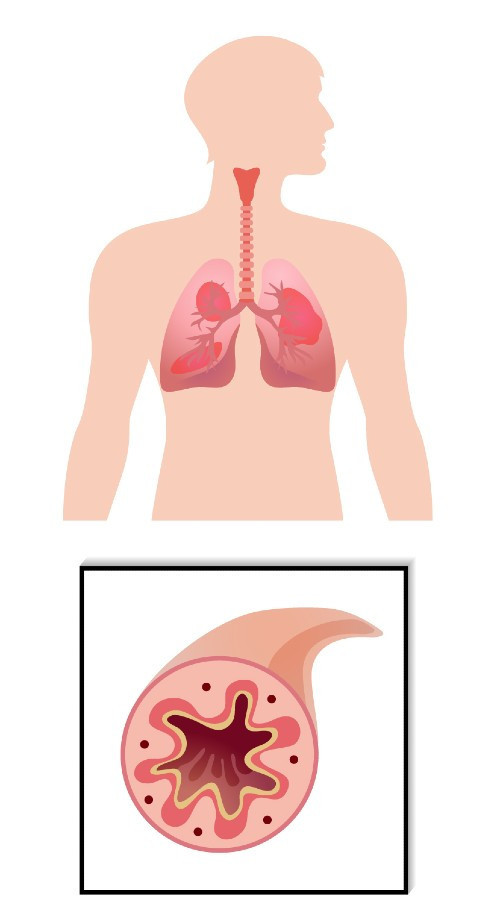
Inflamed Bronchial Tube in Asthma
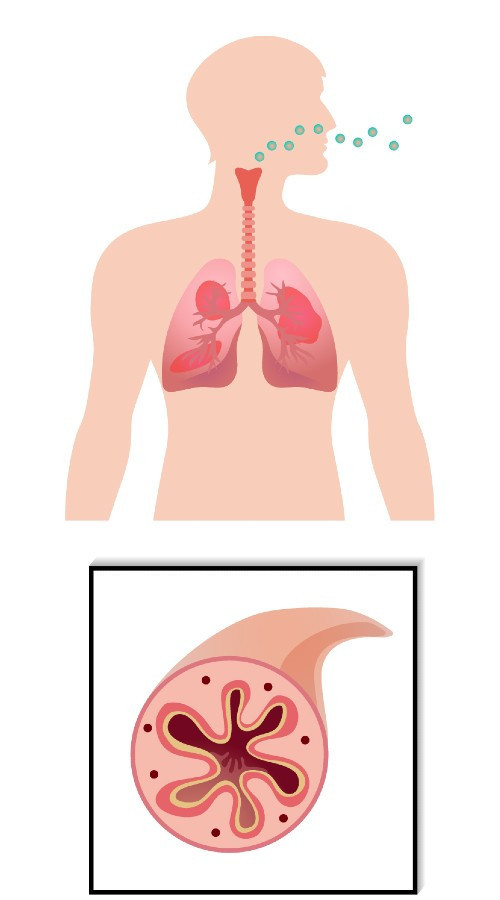
Inflamed Bronchial Tube During in Attack
Common Symptoms
Asthma is characterized by chronic airway inflammation that the airways become narrower and swollen, together with extra mucus produced. Hence it makes the patient difficult to breath and leads to symptoms such as the wheeze, breathlessness, chest tightness and cough. These symptoms may worsen at night or waking, and vary over time. To confirm diagnosis of asthma, spirometry with bronchodilator reversibility testing or twice-daily peak expiratory flow test (PEF) is required to demonstrate the presence of variable airflow limitation.
Risk Factors and Triggers of Asthma
There are a number of risk factors and triggers of asthma. Some common ones are listed below:
| Risk factors | Triggers |
| Family history, allergic condition, smoking, overweight | Allergens (e.g. dust mites, pollens, pet dander), chemical irritants, food, exercise, emotional arousal, cold air, medicine |
Severity of Asthma
The severity of asthma is assessed retrospectively from the level of treatment required to control symptoms and asthma attack. Mild asthma refers asthma that can be controlled by Step 1 or 2 treatment in GINA (Global Initiative Network for Asthma) report, which accounts for approximately 50-75% of all asthma patients. Usually, mild asthma is associated with milder and fewer symptom episodes. However, patients with mild asthma should not ignore the disease as it is still associated with severe exacerbations, which consequently leads to hospitalization or even death. A study showed that in adult patients with mild asthma (symptoms less than weekly in the previous 3 months), 30-37% of them had acute asthma attacks, 16% with near-fatal attacks, and 15-20% died of asthma.
Treatment of Asthma
As asthma is a chronic inflammatory disease with airway constriction, medications for relieving symptoms (bronchodilation) and controlling the root cause (anti-inflammation) are required. Short-acting bronchodilators (SABA) as reliever and inhaled corticosteroid (ICS)-containing regimens, either ICS alone or in combination with long-acting bronchodilators, as controller are usually used in asthma.
SABA has been widely used worldwide since 50 years ago, which provides rapid bronchodilatory effect, within several minutes, to relieve asthma symptoms such as shortness of breath and chest discomfort. While ICS takes weeks to control airway inflammation. Consequently, when SABA and ICS are prescribed as two separate inhalers, the patients tend to use SABA more but avoid ICS, as the former is perceived as effective medicine with rapid symptom relief, while the latter was perceived with no remedial effect but side effects such as oral thrush and hoarse voice. As the patients believe that “my SABA control my asthma well”, they often think additional treatment is unnecessary. Consequently, a number of asthma patients use SABA frequently and some may even become SABA over-reliance (3 cannisters per year). Recent global studies have shown that SABA over-reliance is a common issue worldwide, ranging from 26% - 63% of asthma patients in different western countries. The issue with SABA over-reliance is that as the root cause of airway inflammation cannot be addressed by ICS, the incidence of asthma attack may be elevated.
Realizing the issue, GINA, a globally well-known organization launched in 1993 by a number of international experts in asthma, has no longer recommended SABA alone for asthma treatment since 2019 as solid evidence shows that regular use of SABA makes asthma worse which includes:
- Decreased bronchodilator response, increased allergic response, and increased eosinophilic airway inflammation.
- Using ≥3 canisters/year is associated with higher risk of emergency department admission, while ≥12 canisters/year is associated with higher risk of death
In the meanwhile, GINA recommends to use ICS-containing regimens to reduce risk of asthma worsening and attacks.
Treatment of Mild Asthma
As-needed ICS-formoterol (a fast-onset long-acting bronchodilator, LABA) combination is recommended for mild asthma while low dose ICS should be taken whenever SABA is taken.
Treatment of Moderate-to-Severe Asthma
For moderate-to-severe asthma, ICS-formoterol maintenance and reliever therapy (MART) approach or ICS-LABA plus as-needed SABA is recommended. Patients on MART approach use one single inhaler for both symptom relief and asthma attack prevention, as onset of bronchodilatory effect of formoterol is as fast as SABA, within several minutes, and the effect can last longer, while the ICS component controls airway inflammation at the same time. The advantages of MART approach includes (1) lowering the need of SABA use, (2) the patients achieving both symptom relief and asthma attack prevention in a single inhaler only, and (3) reducing more severe asthma attacks with less overall ICS load versus ICS-LABA plus as-needed SABA.
Treatment of Severe Asthma
For severe asthma, which accounts for about 3-4% of asthma patients, add-on therapies can be considered if the patients have persistent symptoms and/or asthma attacks despite optimized treatment with high-dose ICS-LABA. Add-on options include tiotropium and biologics (e.g. benralizumab, omalizumab) which can further improve lung function and/or reduce severe asthma attacks. Some patients may benefit from low-dose oral corticosteroid (OCS) but long term systemic side effects should be considered.
Common misunderstandings on inhaled corticosteroids (ICS)
Like all other drugs ICS can induce side effects which in general are more likely to occur at higher doses. Common side effects include sore throat, oral thrush and hoarse voice. These side effects can be avoided by rinsing the mouth or cleaning the teeth after ICS medication.
Some asthma patients avoid ICS-containing regimens due to worrisome of systemic side effects such as osteoporosis and thinning of skin. The fact is, unlike oral corticosteroids (OCS), daily dose of ICS used usually low and the sites of action are usually localized to mouth and upper respiratory tract, hence the influences on other organs are usually rare. Having said that, cautions should still be exerted when long term use of high-dose ICS is required.
Some parents are also concerned that use of ICS may affect the body height of their children. Actually, clinical studies show that, though ICS may have some influence on asthma children’s body height, it usually occurs in the first year of treatment and the intensity is small. With moderate doses of ICS, there may be 0.4-1.5cm overall reduction in height as compared with children of the same age. This effect is usually temporary and catch-up occurs in later life.
Hence though ICS has side effects, the risk of poorly treated asthma is far greater than the risk of serious side effects of ICS.